by Bill Blank, M.D.
As many of you know, on March 2, 2015, the Federal Aviation Administration (FAA) initiated a new policy on obstructive sleep apnea (OSA). What is behind this and how will it impact you as a pilot? Here is a little background.
For several years, the National Transportation Safety Board (NTSB) has been concerned about OSA in over the road commercial truckers. There have been several fatal accidents involving truckers who were thought to have had OSA and fell asleep while driving. NTSB reasoned that, if this was a problem among truckers, that it was probably the case with some pilots. Unfortunately, there have been cases (or one case) where flight crews over flew their destinations while both pilots were asleep. In some cases, the undiagnosed sleep apnea of one of the crew members probably was a contributing factor. Because of this the FAA decided to try to identify at-risk pilots. In 2013, the then Federal Air Surgeon, Fred Tilton, tried to implement a program requiring Aviation Medical Examiners (AMEs) to calculate the body mass index (BMI) of pilots. Any pilot with an index of 40 or greater would have been required to have a sleep evaluation by a board certified sleep specialist. Various pilot groups felt that this was expensive overkill and the proposal was withdrawn. Rightfully, the FAA was still concerned about the problem and its potential impact on flight safety. They worked with various groups such as ALPA, AOPA, and EAA to try to develop a more practical, reasonable policy. The March 2 policy change is the result.
As of March 2, your AME is required to make a risk assessment of sleep apnea on each flight physical. Based on your height and weight, the software associated with the 8500-8 form calculates your BMI. The 8500-8 is the form you fill out via “medxpress” and the AME completes and submits electronically to the FAA. An icon has been added for the AME, which he must click on. He cannot submit the form until he has done so. He has six (6) possible options. He must choose one of them.
Applicant Previously Assessed
1. Has OSA diagnosis and is on Special Issuance. Reports to Follow.
2. Has OSA diagnosis and is currently being treated OR has previous OSA assessment. NOT on Special Issuance. Reports to follow.
Applicant Not at Risk
3. Determined to NOT be at risk for OSA at this examination.
Applicant at Risk/Severity to be Assessed
4. Discuss OSA risk with airman and provide educational materials.
5. At risk for OSA. AASM sleep apnea assessment required. Reports to follow.
Applicant Risk/Severity High
6. Deferred, Immediate safety risk. AASM sleep apnea assessment required. Reports to follow.
Most of us will be in category 3. The incidence of OSA is 4-7% in middle-aged people. Number 1 is nothing new. This person already has a Special Issuance and will follow the requirements in it. Number 2 has been diagnosed with OSA, but the FAA does not know about it yet. This could happen if the condition was diagnosed between flight physicals or the pilot (applicant) somehow “forgot” to report it. The FAA is not trying to be punitive. This is an attempt to help you get in compliance without a penalty. You will receive a Special Issuance if qualified. Numbers 4 and 5 are self-explanatory.
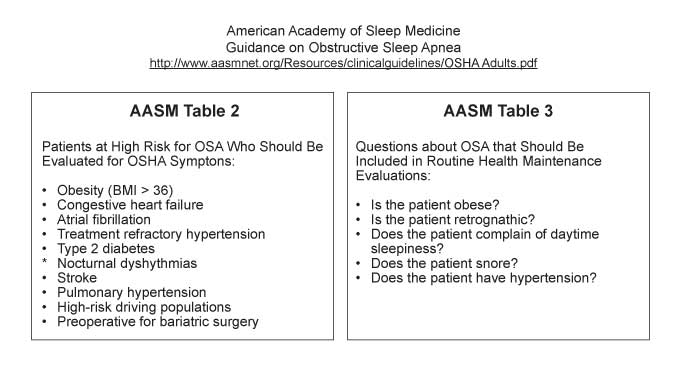
How does the AME decide if the airman is at risk? He will use these tables along with the BMI. A BMI equal to or greater than 40 is considered to be high risk. Between 30 and 40 there is still a significant risk and would probably require selecting choices 4 or 5.
To comply with choice 4, the AME can give you a brochure on OSA published by the FAA. The FAA emphasizes that in almost all cases, the AME should not defer the medical, but issue it. That brings us to choice 6. In this case deferral is mandatory. The FAA feels that only a very small percentage of airmen would fall in this category.
Obviously, we don’t want people falling asleep in the cockpit. There is much more to sleep apnea than aviation safety. It puts us at increased risk for type 2 diabetes, hard to treat hypertension, atrial fibrillation, stroke and many other serious health problems. A contributing factor in the football player Reggie White’s untimely death at 43 was sleep apnea. It is estimated that 80% of people with OSA are undiagnosed. In addition, up to 30% have a BMI of less than 30%.
If you are required to provide information to the FAA regarding a sleep evaluation, you have 90 days to do it. Any physician, including an AME, can do it, but he must follow the guidelines of the American Academy of Sleep Medicine. In many cases an evaluation by a sleep specialist won’t be required.
Suppose you are diagnosed with sleep apnea. If your treatment is successful (and it usually is), using a CPAP breathing system, the FAA will grant you a Special Issuance. At subsequent flight physicals, your AME will be able to issue your medical, providing you bring him documentation of the effectiveness of the treatment and evidence of compliance. This is an AASI (AME Assisted Special Issuance). The FAA will expect you to use the CPAP for an average of 6 hours per night. There are other options besides CPAP, but I don’t have the space to discuss them now. I hope this has been of help. There is much more I could have said, but I didn’t want to put you to sleep.
EDITOR’S NOTE: William A. Blank is a physician in La Crosse, Wisconsin, and has been an Aviation Medical Examiner (AME) since 1978, and a Senior AME since 1985. Blank is a retired Ophthalmologist, but still gives some of the ophthalmology lectures at AME renewal seminars. Flying-wise, Blank holds an Airline Transport Pilot Certificate and has 5300 hours. He is a Certified Instrument Flight Instructor (CFII), and has given over 1200 hours of aerobatic instruction. In addition, Blank was an airshow performer through the 2014 season, and held a Statement of Aerobatic Competency (SAC) since 1987.